The endometrium plays a crucial role in your reproductive health. Its thickness varies throughout your menstrual cycle and life stages, and understanding these changes can help you identify potential issues. Whether you are trying to conceive or experiencing unusual symptoms, knowing what’s normal when it comes to endometrial thickness is essential.
Normal Endometrial Thickness
Your endometrial thickness is not a standard measure. The hormonal changes in a woman’s body throughout the month influence the size and thickness of the endometrial lining. The endometrium is at its thinnest (2-4 mm) during the menstrual cycle (start of the cycle) and grows to 11-12 mm in thickness as the cycle progresses to prepare for pregnancy. If pregnancy doesn’t happen, the endometrial lining shreds back in menstruation; if pregnancy happens, it continues to grow, achieving a maximum size of 14 mm, considered healthy for pregnancy.
Endometrial Thickness During the Menstrual Cycle
- Menstrual phase (days 1–5): The endometrium is at its thinnest, measuring between 2 and 4 mm.
- Proliferative phase (days 6–14): As your body prepares for potential pregnancy, the endometrium thickens to 5-7 mm.
- Ovulation and secretory phase (days 15-28): The endometrial thickness peaks at about 16 mm during the secretory phase, after reaching up to 11 mm before ovulation.
Endometrial Thickness and Pregnancy
When it comes to normal endometrial thickness for pregnancy, a thicker endometrium is generally better. A thickness of at least 7–8 mm is considered optimal for implantation. However, successful pregnancies can occur with thinner or thicker linings, as other factors also play a role in fertility.
Endometrial Thickness after Menopause
After menopause, your endometrium typically measures 5 mm or less owing to decreased oestrogen levels. A thicker endometrium in postmenopausal women can be a cause for concern and may warrant further investigation.
Here’s a quick reference for normal endometrial thickness chart during the different stages:
|
Stage |
Normal Endometrial Thickness |
|
Menstruation (Days 1–5) |
2–4 mm |
|
Proliferative Phase (Days 6–14) |
5–7 mm |
|
Ovulation and Secretory Phase |
Between 11 and 16 mm |
|
Pregnancy |
Around 6 mm |
|
Post-menopause |
5 mm or less |
How is Endometrial Thickness Measured?
Endometrial thickness is typically measured using transvaginal ultrasound. This quick, painless procedure involves inserting a small ultrasound probe into the vagina to visualize the uterus and measure the endometrium at its thickest point.
Causes of Abnormal Endometrial Thickness
Various factors can cause the endometrium to be thinner or thicker than normal. Let’s explore some of the common causes:
Causes of Thin Endometrium
- Oestrogen Deficiency: Low oestrogen levels during the follicular phase can lead to inadequate thickening.
- Age: Older women approaching menopause may have thinner endometrial linings.
- Uterine fibroids or polyps: Noncancerous growths can interfere with endometrial development.
- Anovulation: Irregular or absent ovulation affects oestrogen and progesterone levels necessary for proper endometrial growth.
- Poor blood flow: Inadequate blood flow limits endometrial growth and development.
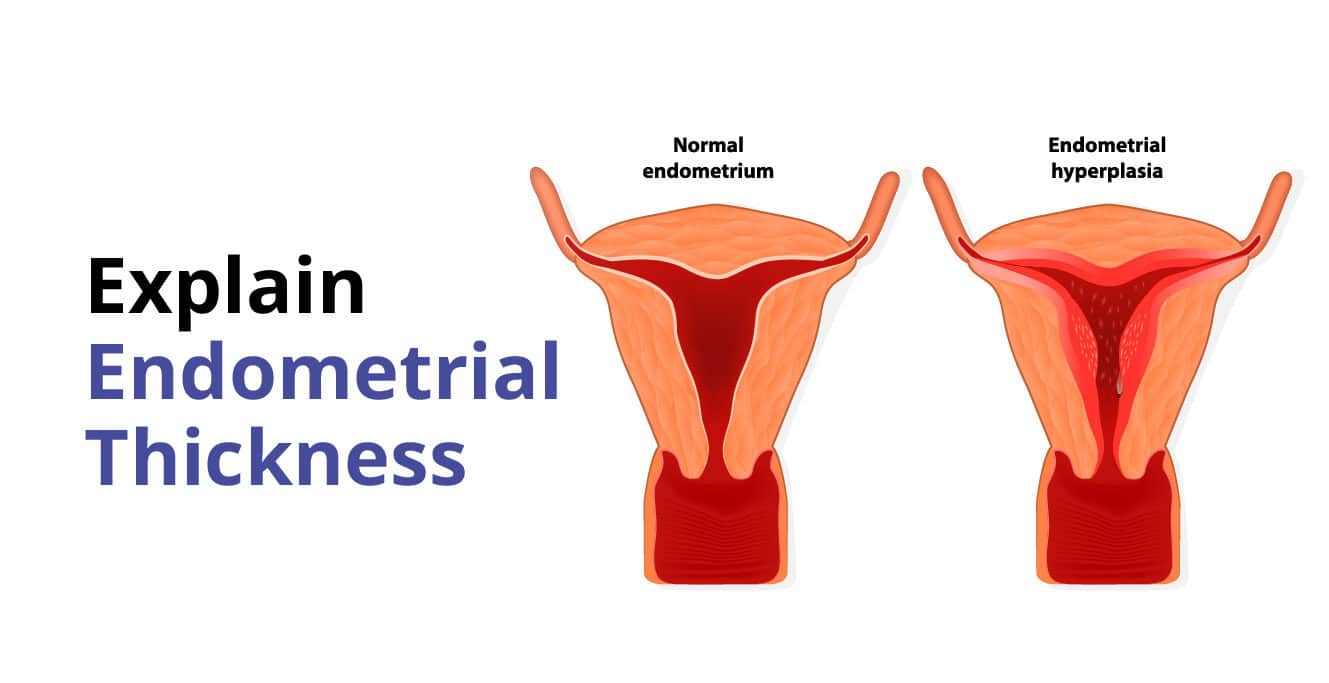
Causes of Thick Endometrium
- Pregnancy: Especially in early pregnancy or ectopic pregnancy.
- Endometrial hyperplasia: Excessive oestrogen and insufficient progesterone can cause thickening.
- Endometrial cancer or ovarian cancer: These conditions can significantly increase endometrial thickness.
- Obesity: Associated with increased endometrial thickness.
- Hormone Replacement Therapy (HRT): Can lead to thickening owing to unopposed oestrogen.
Symptoms of Endometrial Thickness Variations
Symptoms of Thin Endometrium
- Implantation failure and miscarriages: A thin endometrium can lead to difficulties in embryo implantation and early pregnancy loss.
- Irregular menstrual cycles: Women may experience irregular periods, which can manifest as missed cycles or variations in cycle length.
- Light menstrual flow: Menstrual bleeding may be unusually light, sometimes lasting only a short duration (e.g., half a day) with minimal or no clots.
- Painful periods: Some individuals may experience discomfort or pain during menstruation, which can be exacerbated by underlying conditions like chronic endometritis.
- Asymptomatic cases: In some instances, women may not exhibit noticeable symptoms until diagnosed through ultrasound or other medical evaluations.
Symptoms of Thick Endometrium
- Abnormal vaginal bleeding: Heavy or long-lasting bleeding during menstruation, spotting between periods, and bleeding after menopause.
- Irregular menstrual cycles: Cycles lasting less than three weeks or more than five weeks.
- Pelvic pain: Unexplained pelvic pain could be a sign of underlying issues such as endometrial cancer.
Treatments for Abnormal Endometrial Thickness
Treatment for abnormal endometrial thickness depends on the underlying cause and the severity of the condition. Options may include:
Treatments for Thin Endometrium
- Oestrogen therapy: This treatment aims to stimulate endometrial growth. Oestrogen can be administered in various forms, including pills, patches, or injections, and helps to thicken the endometrial lining.
- Human chorionic gonadotropin (hCG): Administering hCG can support implantation after embryo transfer. This hormone mimics the natural hormonal changes that occur during early pregnancy, promoting a suitable environment for the embryo.
- Medications and supplements: Certain medications and supplements can enhance blood flow to the uterus, which is essential for nourishing the endometrial lining. Improved circulation may help in thickening the endometrium.
Treatments for Thick Endometrium
- Progestin: This hormone therapy is commonly used to counteract the effects of excessive oestrogen, which can lead to endometrial hyperplasia (thickened endometrium). Progestin helps regulate the menstrual cycle and can prevent further thickening of the uterine lining.
- Hysterectomy: In severe cases where other treatments have failed or if there is a risk of cancer, a hysterectomy may be necessary. This surgical procedure removes the uterus entirely, eliminating any potential for future complications related to thickened endometrium.
- Pills and vaginal creams: These treatments contain hormones that help regulate the endometrial lining. They can be effective in managing symptoms associated with thickened endometrium and restoring hormonal balance.
- Intrauterine devices (IUDs): Hormonal IUDs can deliver progestin directly to the uterus, helping to thin out an overly thickened endometrial lining and manage bleeding symptoms effectively.
Importance of Endometrial Thickness in Fertility and Pregnancy
Endometrial thickness plays a vital role in fertility and pregnancy:
- Optimal thickness for IVF: An endometrial thickness of 7–10 mm is considered optimal for achieving favorable outcomes during IVF. This thickness ensures that the uterine lining is adequately prepared to support an embryo’s implantation and subsequent development.
- Successful implantation: A properly developed endometrium—neither too thin nor excessively thick—is essential for successful embryo implantation. An ideal thickness allows for sufficient nutrient supply to the embryo while also providing a suitable environment for its growth.
Myth: Endometrial Thickness Is Only Important During Fertility Treatments
Fact: Even outside of fertility treatments, maintaining a healthy endometrial thickness is important for regular menstrual cycles and overall uterine health. Abnormal thickness may also indicate other health issues, such as polyps, fibroids, or endometrial hyperplasia, which should be evaluated by a doctor.
A Word from the Expert
Endometrial thickness is a key indicator of reproductive health, and it’s important for women to be aware of what’s normal for them. Regular check-ups and open communication with your doctor can help you stay on top of any changes and address issues promptly ~ Prachi Benera