Key Takeaways
- Uterine fibroids are non-cancerous tumours in and around the uterus
- Affecting up to 70% of women by age 50 years, these fibroids vary greatly in size, from tiny to as large as a fully-grown foetus.
- Larger fibroids cause heavy menstrual bleeding, pelvic pain, an expanded uterus, and therefore may cause fertility issues.
- Untreated, they may lead to deep vein thrombosis (DVT) & pulmonary embolism.
- Treatment decisions are based on symptoms rather than size.
- Uterine fibroid embolisation (UFE) is a preferred modern treatment option.
- Regular monitoring and maintaining overall health are crucial for early detection and prompt treatment of fibroids.
Introduction:
For many women, the journey to motherhood can be filled with unexpected challenges. One such obstacle that often flies under the radar is uterine fibroids. These non-cancerous growths develop in or on the walls of the uterus, and while many remain small and asymptomatic, larger fibroids can pose significant health risks and impact daily life.
By the age of 50 years, as many as 70% of white women and 80% of African American women may develop fibroids? Despite their prevalence, the conversation around fibroids, especially those that are deemed dangerous because of their size, is often lacking. So, let’s dive deeper into this important topic and arm ourselves with the knowledge needed to navigate this condition effectively.
Interesting Insight!
Did you know that fibroids are more prevalent among South Asian women, including Indian women, compared to other ethnic groups? This is due to a mix of genetic and environmental factors. In fact, nearly 80% of Indian women may develop fibroids by the age of 50 years.
Why Fibroid Size Matters
When it comes to fibroids, size is a critical factor in determining their impact on health. Here’s why:
- Symptom Severity: Larger fibroids are more likely to cause noticeable and disruptive symptoms such as heavy menstrual bleeding, pelvic pain, frequent urination, and reproductive issues.
- Organ Impact: As fibroids grow, they can exert pressure on surrounding organs like the bladder, bowel, and fallopian tubes, leading to discomfort, pain, and potential fertility concerns.
- Treatment Necessity: The size of the fibroid often dictates the necessity and type of treatment required. Larger fibroids may need more intensive interventions, including surgery.
Categorising Fibroids According to Their Sizes
Fibroids come in a range of sizes, each with its own set of potential health implications. Let’s take a look at the different categories:
|
Fibroid Size |
Dimensions |
Description |
|---|---|---|
|
Small |
Less than 5 cm |
Comparable to a pea or lime |
|
Medium |
5-10 cm |
Similar to a peach or large lemon |
|
Large |
More than 10 cm |
Can be as big as a mango or watermelon |
Although small fibroids are generally harmless, their location can sometimes cause issues. Medium-sized fibroids may lead to mild symptoms and pose potential risks to pregnancy and fertility. However, it’s the large fibroids that are considered the most dangerous.
The Danger of Large Fibroids
Which size of fibroid is dangerous, you ask? Fibroids that measure 10 cm (100 mm) or larger are generally deemed more concerning due to potential complications. Small fibroids, typically under 5 cm (about 2 inches), are usually harmless and unlikely to cause significant health issues. However, fibroids over 10 cm (about 4 inches) may require medical attention. Additionally, it’s not just the size that matters; fibroids located near the cervix or fallopian tubes can interfere with fertility or lead to pregnancy-related difficulties, making their position within the uterus just as important to consider.
The reasons why larger fibroids are generally considered dangerous are as follows:
- Pressure on Organs: As fibroids grow larger, they exert more pressure on surrounding organs and nerves, resulting in more severe pain and discomfort.
- Fertility Impact: Large fibroids can distort the shape of the uterus and cause damage to nearby organs, potentially impacting fertility.
- Potential Complications: If left untreated, large fibroids can continue to grow, leading to worsening symptoms, heavier bleeding, and severe cramping.
What Causes Dangerous Fibroids?
Several factors can contribute to the development and growth of dangerous fibroids. These include the following:
- Hormones: Elevated levels of oestrogen and progesterone can fuel fibroid growth.
- Genetics: Family history plays a significant role, with individuals having a higher susceptibility to develop dangerous fibroids if they have a family history of fibroids.
- Diet: An imbalanced diet, particularly frequent consumption of red meat, and a vitamin D deficiency can influence fibroid growth.
- Lifestyle Factors: Obesity, regular alcohol consumption, smoking, and high blood pressure can also affect fibroid size and have health impacts.
Recognising the Symptoms of Dangerous Fibroid
Dangerous fibroids, particularly larger ones, can cause a range of symptoms due to their impact on surrounding organs and tissues.
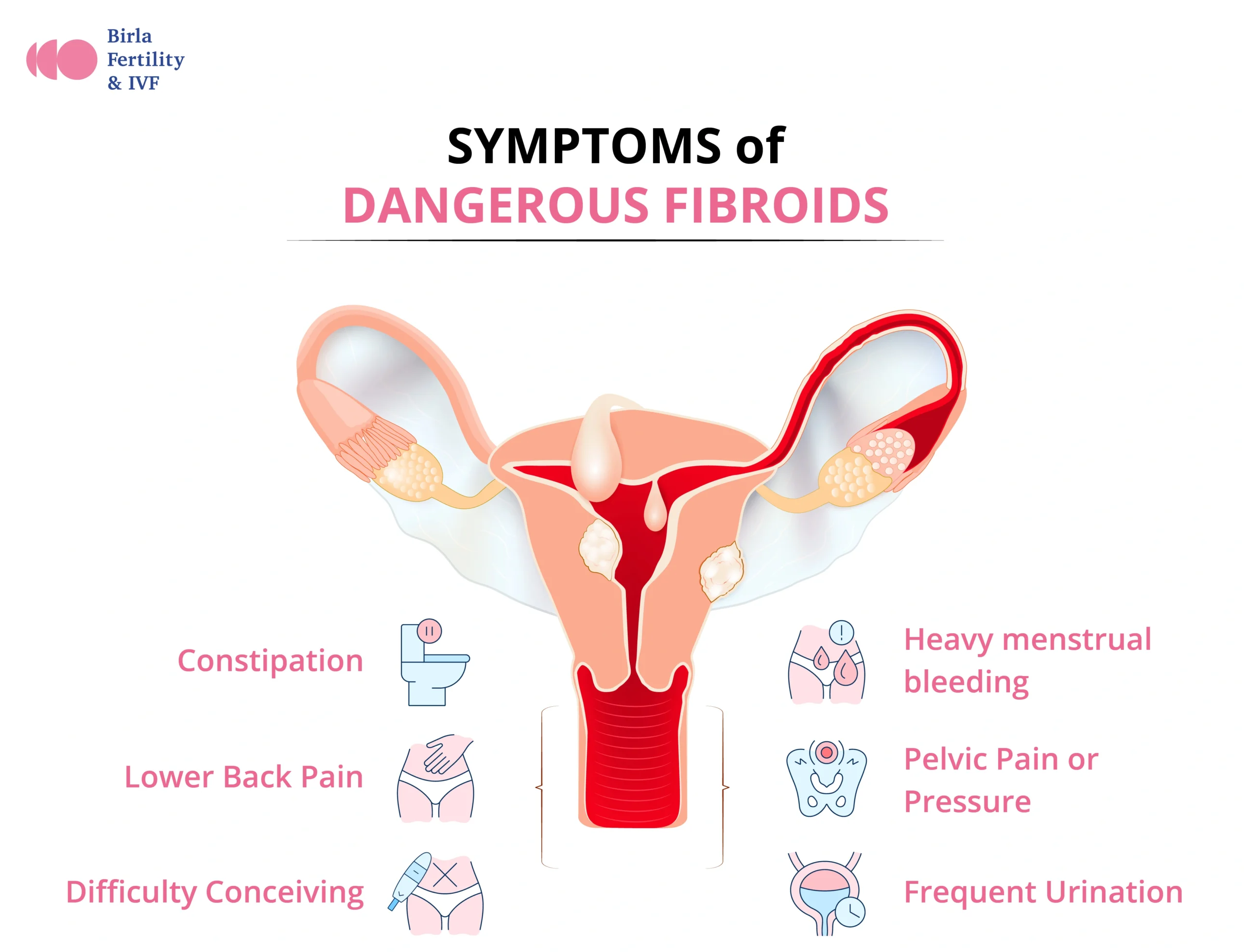
- Heavy menstrual bleeding: Submucosal fibroids within the uterine cavity can lead to excessive bleeding, prolonged periods, clotting, and bleeding between periods. Severe cases may cause iron-deficiency anaemia, leading to fatigue, dizziness, and pale skin.
- Pelvic Pain or Pressure: Large fibroids can create a sense of fullness or pressure in the pelvic area, causing persistent aches or sharp pains that may worsen during menstruation or intercourse, impacting daily life.
- Frequent Urination: Fibroids near the bladder can press against it, reducing its capacity and causing frequent urination, sometimes leading to incomplete emptying and urinary tract infections.
- Constipation: Large fibroids pressing against the rectum can lead to chronic constipation, requiring dietary changes or laxatives to manage.
- Lower Back Pain: Fibroids growing towards the back can press on pelvic nerves, causing persistent lower back pain that may radiate down the legs.
- Difficulty Conceiving: Fibroids that distort the uterus or block the fallopian tubes can interfere with fertility and increase the risk of miscarriage.
Diagnosing Dangerous Fibroids
On the basis of the symptoms, if you suspect you may have a large or dangerous fibroid, the next step is to schedule an appointment with a gynaecologist for a professional diagnosis and discussion of treatment options. Your doctor will typically recommend the following diagnostic steps:
- Imaging Techniques: Ultrasounds are commonly used to detect and measure fibroids. In some cases, MRIs may be necessary for a more detailed view.
- Pelvic Exam: A thorough pelvic exam can help identify fibroids and assess their size and location.
- Symptom Evaluation: Doctors will evaluate symptoms such as heavy menstrual bleeding, pelvic pain, and pressure on the bladder or bowel to determine the presence and impact of fibroids.
It is important to follow any prescribed treatment plan to manage symptoms while awaiting further treatment.
Treatment Options for Dangerous Fibroids
What People Ask…
When should fibroids be removed?
The decision to remove fibroids depends on factors such as:
-
Size: Fibroids larger than 10 cm are often recommended for removal due to potential complications.
-
Symptoms: Fibroids causing severe symptoms should be considered for removal.
-
Location: Fibroids that affect fertility or interfere with pregnancy may need removal.
-
Growth Rate: Rapidly growing fibroids may need intervention, as they could indicate malignancy.
When it comes to treating or removing dangerous fibroids, several surgical and minimally invasive options are available, each with unique benefits and considerations. Here’s a more detailed look at these options:
Surgical Options
- Myomectomy: Myomectomy involves the surgical removal of fibroids from the uterus, preserving the uterus itself. It’s a preferred option for women who wish to retain their fertility or avoid a complete hysterectomy.
-
Types of Myomectomy:
-
Abdominal Myomectomy: Involves an incision in the abdomen to access and remove fibroids, typically chosen for larger or multiple fibroids.
-
Laparoscopic Myomectomy: Uses smaller incisions and a laparoscope (a thin, flexible tube with a camera) to remove fibroids, often resulting in shorter recovery times. However, this approach may not be suitable for very large fibroids.
-
Hysteroscopic Myomectomy: Involves inserting instruments through the vagina and cervix to remove fibroids within the uterine cavity, ideal for submucosal fibroids (fibroids within the inner lining of the uterus).
-
-
Risks and Considerations:
-
Risk of Recurrence: While effective, fibroids may regrow over time, necessitating further treatment.
-
Power Morcellation: A technique sometimes used in laparoscopic myomectomy where the fibroid is broken down into smaller pieces for removal. This method has been linked to the risk of spreading undiagnosed uterine cancer and is not recommended for all patients. Some hospitals now use containment bags to reduce this risk.
-
- Hysterectomy: A hysterectomy is the complete removal of the uterus and is often recommended for women with severe symptoms or for those who have completed their family planning.
-
Types of Hysterectomy:
-
Total Hysterectomy: Involves removing the uterus and cervix, sometimes extending to the ovaries and fallopian tubes.
-
Subtotal (Partial) Hysterectomy: Removes the upper part of the uterus, leaving the cervix intact.
-
Radical Hysterectomy: This more extensive surgery removes the uterus, cervix, part of the vagina, and surrounding tissues, usually reserved for cases where there is a high risk of cancer.
-
-
Risks and Considerations:
-
Irreversibility: A hysterectomy permanently removes the ability to conceive, so it is usually considered when other treatments have failed, or the fibroids are extremely large.
-
Surgical Recovery: Recovery from a hysterectomy can be longer than from other procedures, often requiring several weeks of limited activity.
-
Minimally Invasive Options
Uterine Fibroid Embolisation (UFE)
UFE is a non-surgical procedure where a doctor blocks the blood supply to the fibroids, causing them to shrink and eventually die. A catheter is inserted through a small incision in the groin or wrist, through which tiny particles are injected into the arteries supplying the fibroids.
-
Benefits:
-
Preservation of Uterus
-
Minimal Scarring
-
-
Risks and Considerations:
-
Not Recommended for All Fibroid Types: UFE may not be suitable for women who have large, calcified fibroids or who wish to become pregnant, as it can affect the blood flow to the uterus.
-
Potential for Fibroid Regrowth: In some cases, fibroids may regrow after UFE, especially if the procedure does not target all blood vessels feeding the fibroid.
-
Consulting a gynaecologist or a fibroid specialist is essential to determine the most suitable approach based on individual circumstances.
Word from An Expert
Fibroids are incredibly common, but when they grow to a dangerous size, they can significantly impact a woman’s quality of life and reproductive health. If you’re experiencing symptoms or have concerns about fibroid size, don’t hesitate to reach out to your healthcare provider. With the right diagnosis and treatment plan, it’s possible to find relief and protect your well-being. ~ Dr. Anupam Kumari