Pituitary Tumors: Everything You Need to Know

Table of Contents
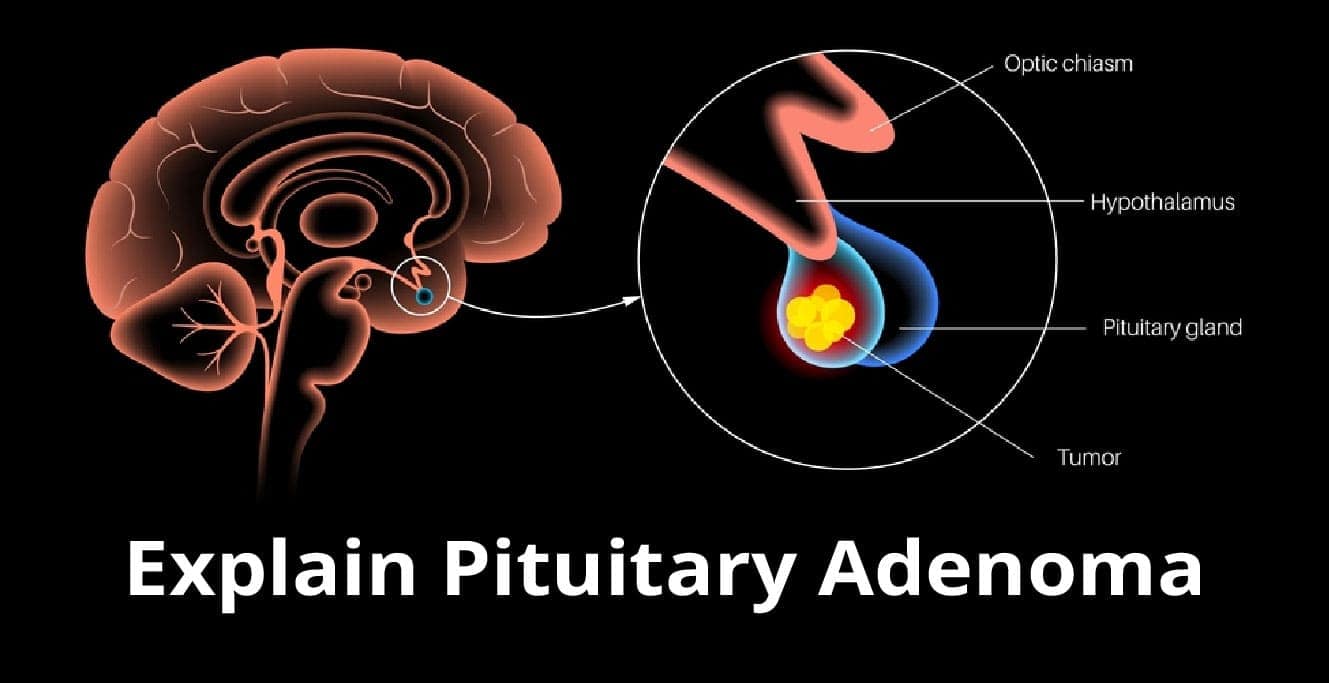
Pituitary tumours affect the pituitary gland, which is located at the brain’s base. The pituitary gland produces hormones responsible for regulating many processes in the body, such as growth, development, and reproduction.
Tumours can occur independently or with conditions such as craniopharyngioma or Rathke’s cleft cyst.
What is a pituitary tumour?
The pituitary gland is a pea-sized located at the base of the brain. It’s sometimes called the master gland because it controls many other glands in the body. It makes hormones that regulate growth, blood pressure, reproduction, and many other important functions.
A pituitary gland tumour may be benign or malignant, but both can cause problems with hormone production. It may cause overproduction or underproduction of one or more hormones, leading to additional problems.
For example, if a person has an overproduction of thyroid stimulating hormone (TSH), this could lead to too much thyroid hormone, which can lead to shaking (tremor) and weight loss, among other symptoms.
Causes of Pituitary Tumours
The exact cause of pituitary tumours is unknown. Still, several risk factors may contribute to their development, including family history, certain genetic conditions, and exposure to certain chemicals or radiation.
Genetic testing can help identify those with a greater chance of developing this tumour.
Symptoms
The main symptoms include vision changes, headaches, changes in hormone levels (such as increased thirst), enlarged sella turcica (the bony cavity near the pituitary gland), or problems with heart function such as high blood pressure.
The most common pituitary tumour symptom is headache. Other symptoms include visual changes, nausea and vomiting, fatigue, and irregular periods. If it is large enough, it can cause problems with urination and constipation.
In some cases, pituitary tumours can cause hormone imbalances, leading to other symptoms like weight gain or loss, excessive thirst or hunger, and changes in mood or behaviour.
As with any other health condition, it’s important to consult your doctor if you experience symptoms.
How is a Pituitary Tumour Diagnosed?
The first step in diagnosing a pituitary tumour is a physical exam. Your doctor will also ask you about your medical history and symptoms.
Here are some of the tests that the doctor might prescribe to diagnose.
– Blood and Urine Tests
If it’s unclear what type of tumour you have, your doctor may order one or more tests to figure out what might be causing it.
A comprehensive metabolic panel looks at how well your kidney works and screens for diabetes and kidney disease.
– Brain Imaging
An MRI (magnetic resonance imaging) machine uses strong magnetic fields and radio waves to create detailed pictures of the brain.
A CT (computed tomography) scan uses X-rays to make cross-sectional images of different body parts, including the brain.
– Vision Testing
If vision problems are a symptom of your condition, it’s important to get an eye exam done as soon as possible.
Eye exams often include testing with an ophthalmoscope, which shines light into the back of the eye and provides a magnified view on a screen to detect any abnormalities.
Doctors may also do retinal scans with an MRI or OCT (optical coherence tomography).
– Genetic Testing
If no other cause for your condition has been found, your doctor may recommend genetic testing.
Treatment options for pituitary tumours
If you have a pituitary tumour, your treatment options will depend on the size and type of tumour and your overall health.
Medication
Hormones, steroids, and anti-seizure medications may be used to control the symptoms of a tumour. These are usually given intravenously or in pill form. Hormone therapy is typically used to reduce a tumour’s size and stop it from growing.
Anti-seizure medication may be prescribed for people with pituitary tumours that produce excessive amount of hormones or in the case of tumours triggered by seizures.
Endoscopic transnasal transsphenoidal approach
An endoscopic transnasal transsphenoidal approach may be more suitable in cases where traditional surgical approaches are not possible due to the tumour’s location, such as when it extends into the sinuses or nasal cavity.
In this procedure, a narrow tube with a camera at its tip is inserted through the nose and into the sinuses.
Transcranial approach
In rare instances, a transcranial approach may surgically remove part of the tumour.
As a result, there is no visible scar on the skin, and patients typically recover much faster than they would from traditional surgery methods.
Radiation therapy
In some cases, radiation therapy is also an option for pituitary tumours. Your doctor may recommend this if the tumour has been deemed too large to remove during surgery safely.
When administered appropriately, radiation therapy helps shrink tumours before surgery or permanently shrinks them after surgery.
Methods of radiation therapy may include:
- Stereotactic Radiosurgery
For tumours that cannot be removed by other means, stereotactic radiosurgery may be an option.
With this technique, high-energy radiation beams are aimed precisely at the tumour to kill cancer cells while minimizing damage to healthy tissues.
- External Beam Radiation
Traditional external beam radiation may be another option, but it has greater risks of side effects like hair loss.
However, new types of external beam radiation called intensity modulated radiation therapy (IMRT), or 3D conformal radiotherapy (3DCRT) allow doctors to deliver higher doses of radiation in a focused area to treat cancer without damaging nearby tissue and organs.
IMRT and 3DCRT are often used for treating pituitary tumours because they limit side effects like hair loss.
Intensity Modulated Radiation Therapy
As mentioned above, IMRT is a newer form of external beam radiation therapy that provides a higher dose of radiation in a tightly controlled area. It’s typically used for treatments involving tumours near sensitive areas such as the eyes, brainstem, and spinal cord.
Patients who undergo IMRT experience fewer side effects than those who receive traditional forms of external beam radiation like 3DCRT or 3Dconformal radiotherapy.
- Photon Beam Therapy
Photon beam therapy is a specialized radiation treatment that uses photons instead of X-rays to treat cancerous cells.
Photons are particles of light energy that can travel very long distances without being absorbed or scattered by atoms in their path, which allows them to reach deep inside the body and destroy any abnormal tissue it encounters.
Surgery
Pituitary gland surgery aims to remove all or most of the tumours. A surgeon may be able to do this by making an incision in your forehead and removing the tumour through this incision.
Endoscopic techniques can also be used with small tumours that may not require surgery.
Conclusion
Pituitary tumours are generally benign but can cause serious health problems if untreated. If you have a pituitary tumour, you’ll likely need surgery to remove it. In some cases, you may also need radiation therapy or hormone therapy.
Birla Fertility and IVF Clinic has a team of experts who can diagnose and treat pituitary tumours. Book an appointment with Dr. Shilpa Singhal today.
FAQs
1. Is a pituitary tumour serious?
Although most pituitary tumours are benign or noncancerous, some can grow and press on nearby structures. This pressure can cause serious health problems, such as vision loss or hypopituitarism, so if you detect any symptoms, see your doctor for an evaluation.
2. What happens when you have a pituitary tumour?
Pituitary tumours are usually benign, but they can cause serious health problems if they grow large enough to press on nearby structures in the brain. Symptoms of a pituitary tumour may include headaches, visual problems, changes in hormone levels, and abnormal growth (in children).
3. Is a pituitary tumour considered cancer?
Most pituitary tumours are noncancerous, meaning they don’t spread to other body parts. However, some pituitary tumours can be cancerous and spread to other tissues. The most common type of cancerous tumour is prolactinoma, which produces too much prolactin hormone.
Our Fertility Specialists
Related Blogs
To know more
Birla Fertility & IVF aims at transforming the future of fertility globally, through outstanding clinical outcomes, research, innovation and compassionate care.
Had an IVF Failure?
Talk to our fertility experts

 Our Centers
Our Centers