What is Hemochromatosis? Causes, Symptoms & Treatment

Table of Contents
- What is Hemochromatosis?
- Symptoms of Hemochromatosis:
- When Do Symptoms Typically Appear?
- How Does Hemochromatosis Affect Body Organs?
- Causes of Hemochromatosis:
- How Can Hemochromatosis Be Diagnosed?
- Treatment for Hemochromatosis:
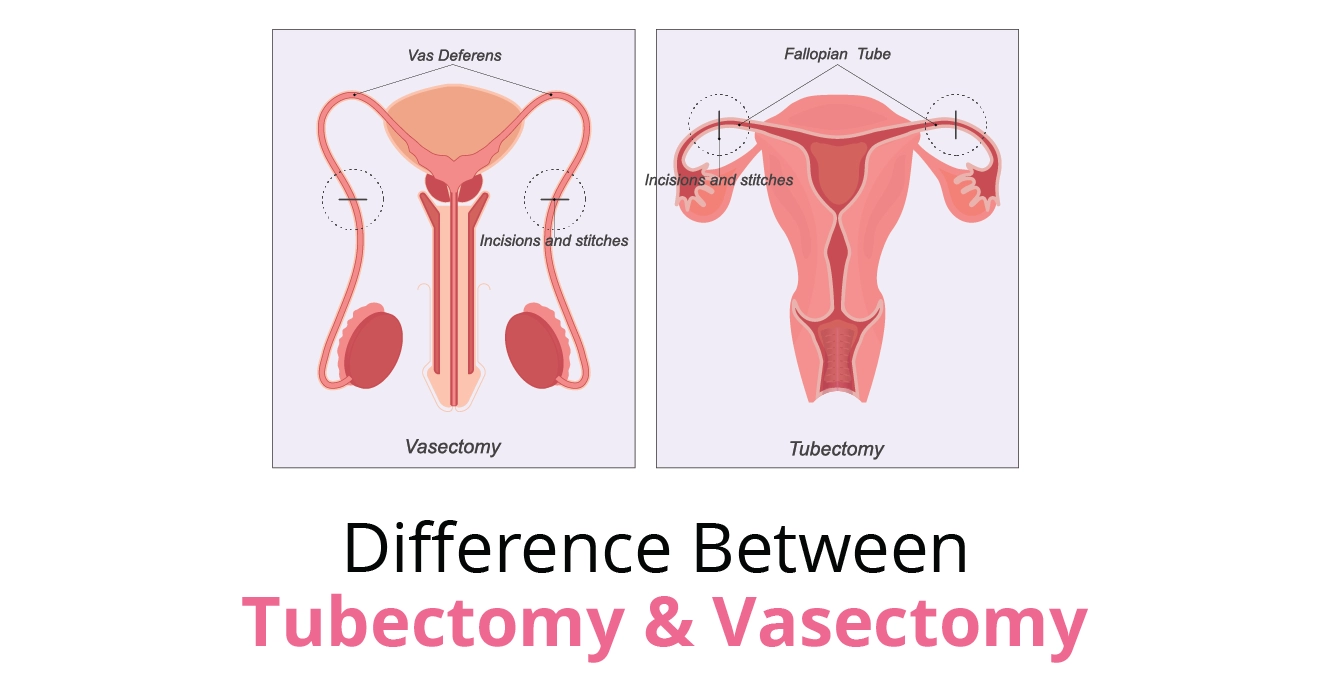
- The Relationship Between Hemochromatosis and Fertility
- Lifestyle Modifications After Hemochromatosis Diagnosis
Imagine your body absorbing more iron than it needs—day after day, year after year—until it starts to overload your organs. That is what happens in hemochromatosis, a condition that often goes unnoticed until it starts causing real damage. Many people do not even realise they have it until they experience symptoms like constant fatigue, joint pain or changes in skin colour. But do you know that early diagnosis and simple treatments can prevent serious complications? Let’s explore what hemochromatosis is, how it affects the body, and what you can do to manage it.
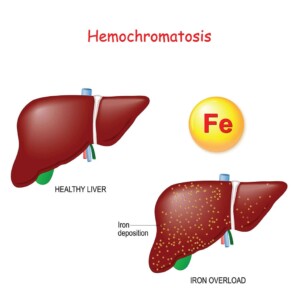
What is Hemochromatosis?
Hemochromatosis is a disorder where the body absorbs too much iron from food, leading to iron overload. Since the body has no natural way to eliminate excess iron, it gets stored in organs like the liver, heart and pancreas causing long-term damage. There are two main types: hereditary hemochromatosis caused by genetic mutations and secondary hemochromatosis which results from conditions like chronic liver disease or frequent blood transfusions. Symptoms develop gradually, often later in life, and can lead to serious complications like liver disease, diabetes, and heart problems. However, with early diagnosis and proper management, the condition is treatable.
Primary (Hereditary) Hemochromatosis:
It is majorly hereditary and is a result of genetic factors. The hemochromatosis gene, or the HFE gene, lives on the short arm of chromosome 6. An individual suffering from primary hemochromatosis usually inherits a copy of the flawed gene from each parent. However, not everyone who has the defective gene develops the condition.
Depending on the onset of primary hemochromatosis, it can be further divided into four types:
- Type 1: It is the most common form of primary hemochromatosis and begins in adulthood
- Type 2: It is also known as juvenile-onset disorder and begins in childhood; sometimes it can also begin as late as 20 years old
- Type 3: This is the intermediate type and generally begins somewhere between the age range of type 1 and type 2
- Type 4: This is very similar to type 1 and begins between the ages of 40 and 60
Secondary Hemochromatosis:
This type arises due to external factors or other medical conditions that cause iron overload. Causes include:
- Liver Diseases: Conditions like hepatitis C or fatty liver disease can disrupt iron metabolism.
- Alcohol Consumption: Chronic alcohol intake can increase iron absorption and exacerbate liver damage.
- Frequent blood transfusions – Common in conditions like thalassemia or sickle cell disease, where repeated transfusions increase iron levels.
- Iron-loading anaemias – Disorders like aplastic anaemia or sideroblastic anaemia cause the body to absorb too much iron.
- Excessive iron supplements – Long-term intake of high-dose iron supplements or injections can lead to iron overload.
- Long-term kidney dialysis – Dialysis patients may experience iron accumulation due to repeated blood transfusions and altered iron metabolism.
Symptoms of Hemochromatosis:
Symptoms of type 1 hemochromatosis, the most common kind, begin between the age range of 30 and 60. Studies reveal that men tend to develop symptoms earlier than women. Women often do not experience symptoms until menopause.
Some of the initial hemochromatosis symptoms are:
- Joint pain
- Sudden weight loss
- Weakness and fatigue
- Nausea
- Fever
- Erectile dysfunction
- Irregular period
As the condition advances, the hemochromatosis symptoms can worsen.
- Low libido or complete loss of sexual drive
- Skin darkening
- Yellowing of eyes and skin
- Chest pain
- Difficulty breathing and shortness of breath
- Stiff joints and fingers
- Testicles getting small
- Frequent urge to pee
- Frequent thirstiness
- Abdominal pain
- Abdominal swelling
- Memory fog
- Heart failure
- Diabetes
- Loss of body hair
When Do Symptoms Typically Appear?
Hemochromatosis symptoms often manifest later in life:
Men
Symptoms of hemochromatosis typically appear after age 40 when excess iron starts affecting organs. Since men do not lose iron naturally, it accumulates faster, leading to fatigue, joint pain, and liver issues earlier in life.
Women
In women, symptoms usually develop after age 60 or post-menopause. Menstruation and pregnancy help regulate iron levels, delaying buildup. In case these natural iron losses stop, symptoms like fatigue, irregular periods, and joint pain may emerge.
How Does Hemochromatosis Affect Body Organs?
Excess iron deposition can impact various organs:
- Liver: Excessive iron can lead to cirrhosis or liver cancer.
- Heart: Iron overload can cause arrhythmias and heart failure.
- Pancreas: Too much iron may result in diabetes mellitus.
- Joints: Iron overload can lead to arthritis.
- Endocrine Glands: A high quantity of iron can affect glands like the thyroid and pituitary, leading to hormonal imbalances.
Causes of Hemochromatosis:
Family History
Primary hemochromatosis, which is hereditary hemochromatosis, is caused by gene mutations. If an individual inherits the HFE gene from each parent, hemochromatosis is caused. The HFE gene has two common mutations, namely, C282Y and H63D.
If an individual inherits both the genes, i.e., C282Y and H63D, the chances of developing the condition are very high. However, if an individual inherits only one of the mutated genes, they are unlikely to develop the condition.
The individual can still pass the gene to their child. However, the child will only develop the condition when an abnormal gene has been inherited from the other parent as well.
Ethnicity
Studies reveal that people of Northern European ethnicity are more prone to developing hemochromatosis. In the United States of America, 1 in 300 non-Hispanic white people has hereditary hemochromatosis. People with Asian, Hispanic, and Black ethnicities are less prone to hemochromatosis.
Gender
Women undergo iron loss during the menstruation cycle; hence, they are less likely to develop hemochromatosis than men. During pregnancy, too, women’s bodies store fewer vitamins and minerals. Men are more likely to develop symptoms of hemochromatosis by the early or late 30s.
How Can Hemochromatosis Be Diagnosed?
If your family has a history of hemochromatosis, we advise you to regularly monitor your iron levels even if you are not experiencing symptoms. It is better to diagnose hemochromatosis at an early stage and start taking preventive measures as soon as possible. This way, you will be less likely to develop advanced symptoms in the future.
When you visit a doctor, they will ask about your symptoms and family history. Ensure you are very transparent regarding your family history and other vital information like your predominant diet, any supplements you take, and other health complications. A doctor may carry out some physical exams to diagnose hemochromatosis.
Genetic Testing
DNA and genetic testing will reveal you have inherited the mutated gene from your parents. This is very much like a blood test, where the doctor will draw some blood and collect some cells from your mouth using a cotton swab.
Blood Testing
A TS test, i.e., serum transferrin saturation test, is a blood test that measures the level of iron in your blood. It is not a very reliable testing method to diagnose hemochromatosis, but it does help the doctor understand your condition better.
MRI
Doctors sometimes also suggest non-invasive tests to diagnose hemochromatosis. An MRI scan is one technique that allows them to measure the iron level in your body.
Liver Biopsy
During a liver biopsy, the doctor will extract a small piece of tissue from your liver and check its iron levels. The liver is the first organ in the human body that is affected by excessive iron in the body.
Treatment for Hemochromatosis:
Timely hemochromatosis treatment will allow you to effectively manage your symptoms and other complications. Apart from the medical treatment, the patient will also have to undergo some lifestyle changes like having regular blood checks, avoiding supplements, avoiding alcohol, etc.
Phlebotomy
Phlebotomy is the most common hemochromatosis treatment where your blood is removed regularly to regulate the iron level in the body. It is usually removed three to four times a year.
Chelation Therapy
Chelation therapy involves taking medicine that removes excess iron from your body through excretion. It is not as common as phlebotomy and only done when it is difficult for an individual to have the blood removed regularly due to other health complications.
The Relationship Between Hemochromatosis and Fertility
Iron overload can impact reproductive health in both males and females:
Female Fertility
- Menstrual Irregularities: Iron deposition in the pituitary gland can disrupt hormone production. This may cause irregular periods.
- Early Menopause: Women having hemochromatosis may experience menopause earlier than the normal age range.
- Infertility: Hormonal imbalances in hemochromatosis can hinder ovulation which is a key reason for female infertility.
Male Fertility
- Erectile Dysfunction: Iron accumulation can damage the pituitary gland, leading to reduced testosterone levels and erectile dysfunction.
- Reduced Libido: Lowered testosterone can decrease sex drive.
- Testicular Atrophy: Shrinkage of testicles due to hormonal disturbances.
Lifestyle Modifications After Hemochromatosis Diagnosis
Adopting certain lifestyle changes can help manage iron levels:
- Reduce intake of red meat and iron-fortified products.
- Avoid vitamin C supplements as vitamin C enhances iron absorption.
- Iron overload can weaken your immune system therefore, avoid raw seafood as it can increase the risk of infections.
- Minimise or eliminate alcohol to reduce liver strain.
- Avoid iron supplements including multivitamins containing iron.
Hemochromatosis may feel challenging to manage but you must understand that it is not impossible to manage it. On-time treatment and making small yet impactful modifications in your everyday routine can make a big difference. If you have any concerns, Birla Fertility & IVF is here to help! Our experts are here to support you especially if you are worried about your fertility and overall wellness. All you need to do is follow the right approach with a positive mindset and you can live a healthy life.
Our Fertility Specialists
Related Blogs
To know more
Birla Fertility & IVF aims at transforming the future of fertility globally, through outstanding clinical outcomes, research, innovation and compassionate care.
Had an IVF Failure?
Talk to our fertility experts

 Our Centers
Our Centers