In Vitro Fertilization (IVF) – Procedure, Benefits, Treatment, Do’s and Don’ts

Table of Contents
- What is In Vitro Fertilization (IVF)?
- Steps Involved in IVF Treatment:
- Types of IVF Treatments:
- What is the Cost of IVF Treatment?
- Why is IVF Recommended?
- What is the IVF Success Rate?
- How Do I Prepare Before IVF Treatment?
- What to Do After an IVF Cycle
- Signs of a Successful IVF Cycle:
- Reasons for Failure of IVF Cycle:
- What Should I Avoid After IVF?
- Are There Any Complications With IVF?
- Side Effects of IVF Injections
- How Do I Select an IVF Clinic in India?
- What Questions Can You Ask Your Fertility Specialist?
- Conclusion
- FAQs
- I am 45, can I still undergo IVF treatment?
- How long does it take IVF to show results?
- Can I conceive through IVF after menopause?
- How long do I have to take off from work for the IVF procedure?
- Is IVF treatment stressful?
- What is the full form of IVF?
- How many injections are needed in an IVF cycle?
- What are the benefits of IVF?
- When should I opt for IVF?
- How many IVF cycles should a woman try?
In vitro fertilization (IVF) has turned out to be a massive breakthrough in India. It’s been more than 4 decades now since the first IVF baby was born. With that baby, a ray of hope was introduced to reproductive medicine. Infertility treatments have evolved over time and become safer, more effective, and more successful.
What is In Vitro Fertilization (IVF)?
IVF stands for “in vitro fertilization.” This is a medical procedure used to help individuals or couples who are struggling with infertility conceive a child. In this process, fertilization of an egg and sperm occurs outside the body, in a laboratory dish or test tube (hence the term “in vitro,” which means “in glass” in Latin). Once the embryos are formed, they are transferred back into the woman’s uterus, with the hope that they will implant and develop into a successful pregnancy.
The IVF process involves several steps. Initially, the woman undergoes hormonal stimulation, followed by different necessary steps to complete the IVF treatment process. During this time, the woman’s response is monitored through ultrasound scans and blood tests.
Steps Involved in IVF Treatment:
In vitro fertilization (IVF) is a complex reproductive technology that helps individuals or couples achieve pregnancy. The IVF process typically involves several steps, but it’s important to note that each clinic may have a different timeline for initiating and executing the procedure based on the patient’s specific fertility needs. The following are the standard steps involved in an IVF cycle:
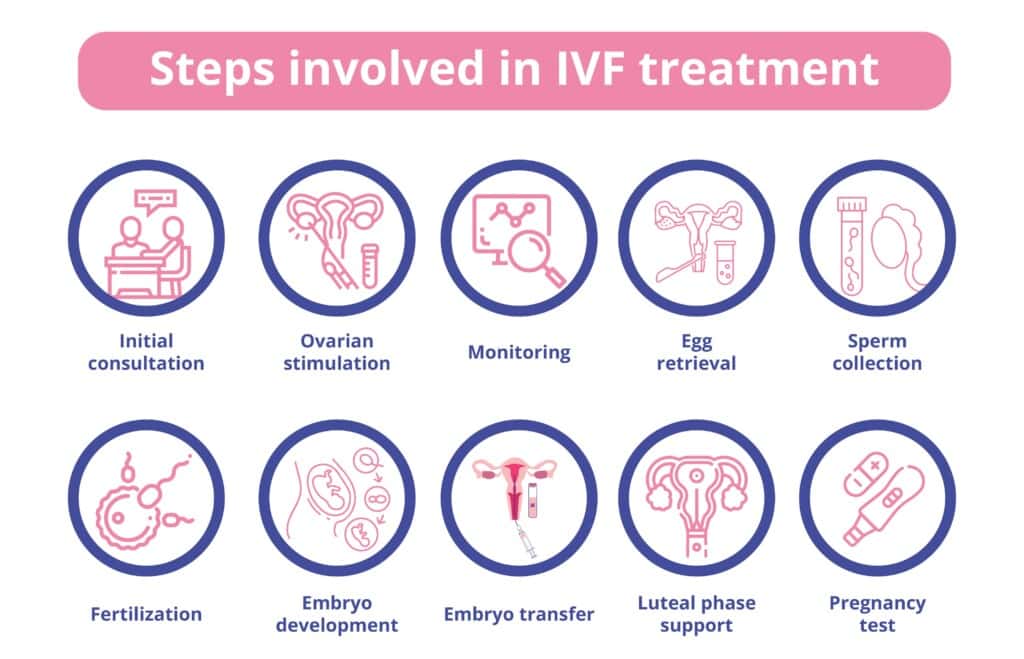
- Initial Consultation: The first step is to consult with a fertility specialist or reproductive endocrinologist. They will review your medical history, conduct various tests, and discuss the potential treatment options available.
- Ovarian Stimulation: During this stage, the woman is given hormonal medicine to stimulate her ovaries into producing several healthy eggs rather than the single egg that develops during a normal menstrual cycle. These drugs are normally taken for 8-14 days and are administered via self-administered injections.
- Monitoring: Throughout the ovarian stimulation phase, regular monitoring is crucial. This involves frequent ultrasounds and blood tests to assess the development of ovarian follicles (fluid-filled sacs containing eggs) and hormone levels.
- Egg Retrieval: An egg retrieval technique is performed once the follicles have achieved the proper size and maturity. Under light anaesthesia, a doctor utilises ultrasound guidance to aspirate fluid and eggs from the ovaries with a thin needle. The treatment takes approximately 20-30 minutes.
- Sperm Collection: When the egg retrieval procedure happens, the sperm donor or male partner is asked to provide the semen sample. Later, the sample is processed in the laboratory to separate the healthy sperm from the seminal fluid.
- Fertilization: In the laboratory, the retrieved eggs are mixed with the prepared sperm. Fertilisation can take place via conventional insemination, in which the sperm is placed close to the eggs, or via intracytoplasmic sperm injection (ICSI), in which a single sperm is directly injected into each mature egg.
- Embryo Development: The fertilized eggs, now called embryos, are cultured in a controlled environment in the laboratory. They are monitored for cell division and growth for several days.
- Embryo Transfer: The developed embryos are put into the woman’s uterus after a period of incubation, typically 3-6 days after retrieval. The technique is normally painless and does not necessitate the use of anaesthesia. The number of embryos transferred is usually decided by criteria such as the woman’s age, the quality of the embryos, and previous IVF treatments.
- Luteal Phase Support: Following the embryo transfer, the woman may be prescribed medications (such as progesterone) to support the uterine lining and early pregnancy.
- Pregnancy Test: Approximately 10-14 days after the embryo transfer, a blood test or a urine test is conducted to determine if the woman has conceived a baby. If the test comes back positive, it says confirm pregnancy. On the other hand, if the result is negative, that’s a sign of failed IVF treatment process.
It’s worth noting that not all IVF cycles result in pregnancy, and individuals or couples may require multiple attempts before achieving a successful pregnancy. The process can be emotionally and physically demanding, and it’s important to have proper support and guidance from your fertility expert throughout the journey.
Types of IVF Treatments:
IVF is one of the methods of assisted reproductive technology (ART) to help couples with infertility issues. According to the patient’s fertility needs, the IVF technique is determined. Here are the different types of IVF treatments:
- Natural IVF cycle – In a natural IVF (in vitro fertilization) cycle, the aim is to collect the egg that is naturally selected and released by the woman’s body during her natural menstrual cycle. Unlike the traditional IVF cycle, which involves stimulating the ovaries with medications to produce multiple eggs, natural IVF focuses on retrieving the single egg that is naturally developed.
- Minimal stimulation – Minimal stimulation, also known as low stimulation or minimal medicine, is used for IVF treatment. It is a modified approach to in vitro fertilization (IVF) in order to stimulate the ovaries for egg production. The sole aim of minimal stimulation is to reduce the use of medications and minimize the risk of complications. It is also known as mini-IVF or mild stimulation IVF.
In a conventional IVF treatment process, high doses of fertility medications are used to stimulate the ovaries, leading to the development of multiple eggs. However, this approach can be associated with a higher risk of ovarian hyperstimulation syndrome (OHSS) and other side effects. Instead of the daily injections used in conventional IVF, minimal stimulation IVF may involve using lower doses of injectable medications or oral fertility drugs such as clomiphene citrate or letrozole. These medications help stimulate the ovaries to produce a smaller number of eggs.
- IVF with Frozen embryo transfer (FET) – IVF involves the fertilization of an egg with sperm outside the body, in a laboratory setting. After fertilization, the resulting embryos are typically cultured for a few days, and then one or more of them can be transferred to the woman’s uterus in a process known as embryo transfer. FET, on the other hand, stands for frozen embryo transfer. It is a technique used in IVF where embryos not transferred during the initial fresh cycle are cryopreserved (frozen) for future use. These frozen embryos can later be thawed and transferred to the woman’s uterus during a frozen embryo transfer cycle.
- IVF with Elective Single Embryo Transfer (eSET): During this technique of IVF, an expert selects a single embryo from a large number of fertilised eggs. Later, the selected, healthy embryo is implanted in the lining of the uterus to achieve pregnancy.
- IVF with Intracytoplasmic sperm injection (ICSI) – IVF with ICSI (Intracytoplasmic Sperm Injection) is a specialized form of in vitro fertilization (IVF) used to overcome certain types of male infertility. ICSI is primarily recommended when there are significant issues with the quality or quantity of sperm available for fertilization. During the ICSI procedure, a single sperm is selected and directly injected into the cytoplasm of an egg retrieved from the woman. IVF with ICSI has been shown to be highly effective in overcoming male-factor infertility, such as low sperm count, poor sperm motility, or abnormal sperm shape. It provides an opportunity for couples facing fertility challenges to achieve pregnancy and have a child.
- Sperm Collection: A semen sample is obtained from the male partner through masturbation or surgical extraction methods such as testicular sperm aspiration (TESA) or testicular sperm extraction (TESE). To prepare the semen first, the sample undergoes a series of laboratory processes to isolate motile and healthy sperm. This involves separating the sperm from the seminal fluid and selecting the most viable sperm for injection. This step is performed by an expert embryologist, using a specialized microscope and micromanipulation tools, a single sperm is carefully injected into the cytoplasm of each mature egg.
- IVF with Donor Sperm: It is one of the best-known IVF methods for single mothers who want to conceive and raise a baby alone. However, in this technique, a woman is provided with ovarian stimulation medications to prepare for egg retrieval in order to combine with donor sperm for embryo culture.
What is the Cost of IVF Treatment?
The average IVF cost in India may start at Rs. 85,000 and can go as high as Rs. 3,50,000. The above-mentioned cost for IVF in India is an approximate range to give you an idea of the expenses included in the treatment. However, the final cost may differ from one individual to another based on various factors, such as –
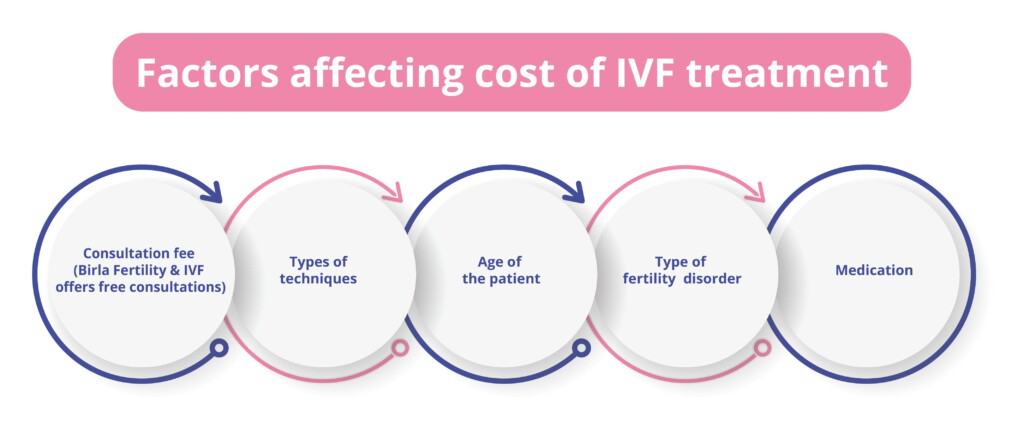
- The consultation fee of a fertility expert (Birla Fertility & IVF offers free consultations)
- The types of techniques used for IVF treatment
- Age of the patient
- The type of fertility disorder
- Medication is given and recommended throughout the IVF treatment
Why is IVF Recommended?
In vitro fertilization (IVF) is the most successful technique among all fertility treatments. Though, typically, the reason and requirements for undergoing IVF may differ from one patient to another. Below are a few causes and reasons for which IVF is advised for male and female partners.
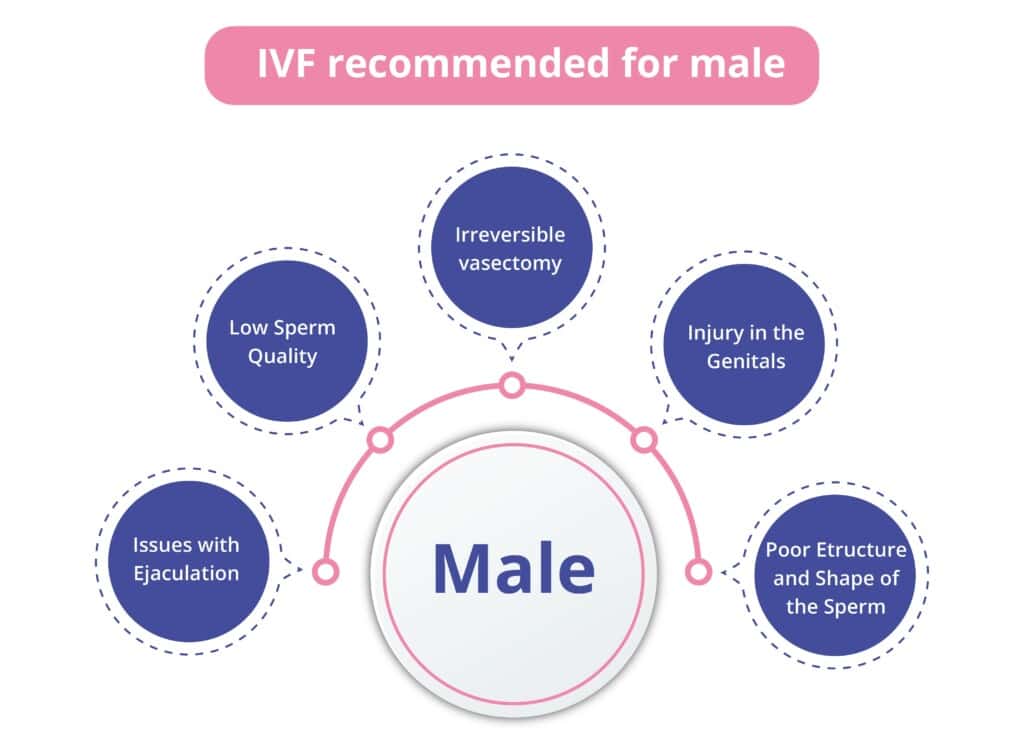
Male Requirements:
- Issues with ejaculation
- Low sperm quality
- Irreversible vasectomy
- Injury in the genitals
- Poor structure and shape of the sperm
- Affected with paralyses, etc.
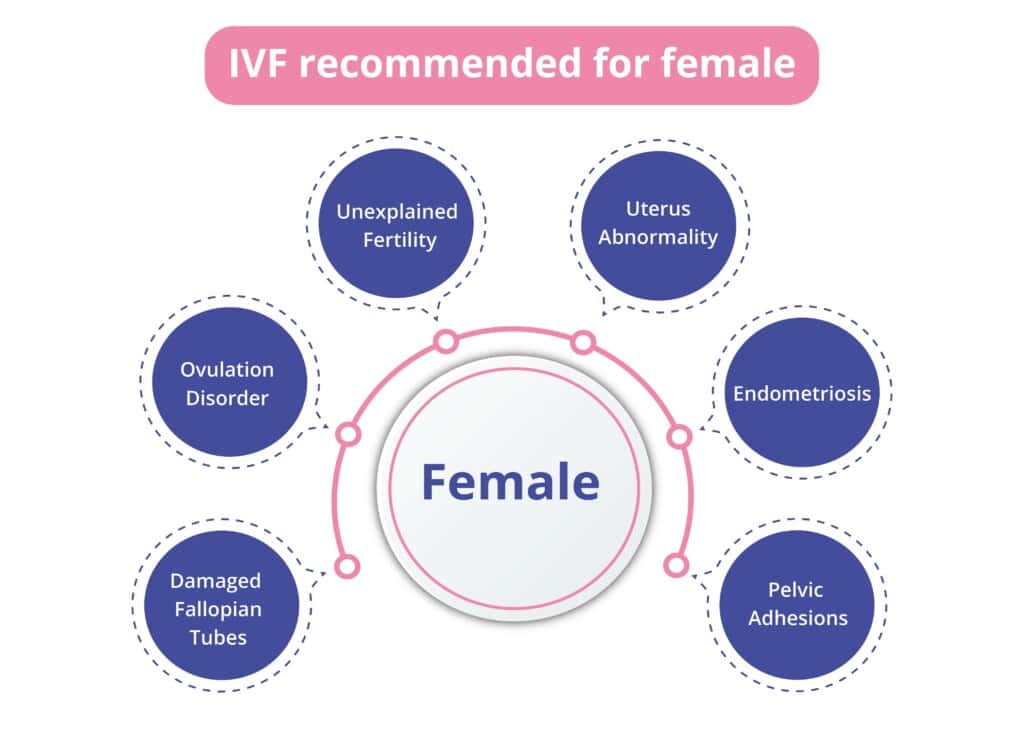
Female Requirements:
- Damaged fallopian tubes
- Ovulation disorder
- Unexplained fertility
- Uterus abnormality
- Endometriosis
- Pelvic adhesions
What is the IVF Success Rate?
According to the reports, the average IVF success rate in India is somewhere between 30% and 35%. However, the success rate of IVF varies based on various factors, including the woman’s age, the type of infertility disorder, the quality of the sperm and eggs, the expertise of the fertility specialist, and the reputation of the fertility clinic from which you are receiving the IVF treatment. At Birla Fertility & IVF the IVF success rate is 85% and for multi-cycle the success rate is 100%. To learn more, contact us at the given number.
IVF success rate is typically given as a percentage of live births per IVF cycle or per embryo transfer. The IVF success rate is often greater for younger women but declines with age. The following IVF success rates are reported according to the female’s age. Though the IVF success rate may differ based on the overall fertility health of the patient. Refer to the below table to get an idea of the success rate by age of IVF treatment.
| Age of the Patient | Average Success Rate |
| Under 35 | 35% – 40% |
| 35 – 37 | 25% – 35% |
| 38 – 40 | 20% – 25% |
| 41 – 42 | 10% – 15% |
| Above 42 | 3% – 8% |
*The above table, comprising success rates as per age, is to give you an idea. However, the outcome may vary depending on factors like IVF technique, comorbidities, weight, and the overall health of the female.*
How Do I Prepare Before IVF Treatment?
It is always a better idea to prepare yourself for IVF treatment. By doing this, you can improve your chances of successful IVF treatment and can expect a smooth journey. Here are a few tips that can help you prepare before undergoing IVF treatment:
- Know the IVF procedure – Learn about the IVF method, including all the stages of the treatment, potential risks, success rates, and any lifestyle adjustments that may be required.
- Consult the fertility expert – It is advisable to schedule your appointment with a fertility specialist. They will run a thorough diagnosis in order to examine the overall fertility health and determine the IVF technique based on the results of the reports.
- Lifestyle modifications – Follow healthy lifestyle practices to elevate your chances of a successful outcome. The lifestyle adjustments may include maintaining an 8 hours sleep pattern, eating a healthy and well-balanced diet that is enriched with nutrients, managing your stress, and quitting drugs, tobacco, and alcohol.
- Pre-genetic testing – Getting a genetic test before IVF treatment can help you eliminate hereditary illnesses or chromosomal abnormalities during embryo culture. The result of such tests can boost the likelihood of a successful pregnancy.
- Budget considerations – You can always discuss your financial considerations with your chosen fertility clinic. Also, fertility treatments like IVF can be expensive, therefore, to combat that, you can figure out loans and aid for the cost strain beforehand to avoid any stress in the future.
- Supplements and medication – Eat your recommended supplements and medications on time to manage your menstrual cycles and stimulate healthy egg production. Supplements like folic acid and prenatal vitamins are advised to boost overall fertility health.
- Join groups – Consider joining groups to manage your stress levels. IVF treatment can be physically and mentally exhausting, therefore, it is better to seek help from your friends, family, and partner.
- Prepare your home – Prepare your home for the IVF process by organizing any medications, supplies, or equipment that you may require. Familiarize yourself with drug storage and administration guidelines.
What to Do After an IVF Cycle
Every patient’s IVF journey is different. Therefore, there are various critical steps one needs to take post IVF treatment. Following are a few general guidelines that can help you take better care of yourself better –
- Rest– Take proper rest after your IVF cycle. It is necessary to take proper rest in order to avoid any sort of exhaustion.
- Sleep pattern– It becomes important to maintain 8 hours of sleep rigorously. Lack of sleep can lead to constant fatigue and also result in stress.
- Light activities– It is better to avoid any type of strenuous activity. Experts advise not to pick up any heavy objects and advise to avoid any physical activities that may put pressure around the pelvis area.
- Follow doctor’s guidelines– After the IVF cycle, it is critical to follow all the instructions given by your fertility specialist. Every case is different, and to avoid any complications and achieve positive outcomes, experts provide a set of tailored guidelines.
- Medications– Take your recommended medications and supplements at the advised time. These medications are given to support the post-embryo implantation process and its development. In addition, if you are feeling any kind of side effect, reach out to your doctor immediately. The doctor will either replace the medicine or may provide a better alternative.
- Lifestyle– Follow the given IVF diet chart and recommendations. Diet has a major impact on the results of the IVF cycle. You should always engage in the recommended light exercise to improve the blood circulation in the body. A healthy diet and proper routine can directly impact the growth of the implanted embryo and lead to a successful pregnancy.
Signs of a Successful IVF Cycle:
A successful IVF cycle is indicated by a few signs mentioned below. These signs are generally a result of successful embryo implantation. Once the cultured embryo is transferred into the uterine wall, you will experience some changes in the body. Here are some signs that indicate successful implantation –

- Tenderness in the breast– Some women may experience swelling, soreness, and tenderness around the areola region of their breasts.
- Discomfort in the pelvis – You may experience mild discomfort or slight pain around the pelvis area. Some doctors also call it implantation cramps because the embryo settles in the uterine cavity and creates space to grow into the uterus.
- Nausea – A female may also experience nausea and vomiting several times during the day. Typically, it is also known as morning sickness.
- Fatigues – There is a possibility you will complain about the constant fatigue and feeling of tiredness because of the changes in hormone levels and the progress of pregnancy.
- Vaginal discharge – You will notice changes in your vaginal discharge post-IVF cycle. Doctors report that it occurs due to changes in the body.
- Spotting or light bleeding – This is known to be one of the significant signs that indicate a positive pregnancy. This is also called implantation bleeding and commonly happens for a week after 2 weeks of implantation.
- Missed menstruation – Missing periods after implantation can be a sign of a successful implantation, which also means that the implantation can progress to a confirmed pregnancy.
Reasons for Failure of IVF Cycle:
Several reasons can result in a failed IVF cycle. There are various factors that can also affect the final result of the IVF treatment. The below mentioned are a few reasons that can lead to failed IVF cycles –
- Sperm-related disorders – If the quality of the sperm is poor, the count of sperm is low, and the sperm are abnormally structured are a few reasons that can result in the failure of the IVF cycle.
- Quality of cultured embryo – If the cultured embryo is of poor quality, it does not develop favourably and may result in chromosomal abnormalities.
- Implantation failure – It is one of the critical and complex steps of the IVF cycle, and at times the selected embryo fails to implant successfully into the uterine lining, leading to failed IVF cycle.
- Uterine abnormalities – This can turn out to be a significant factor that can affect the success chances of IVF results. Uterine abnormalities such as a thin wall or endometrium can directly impact implantation.
- Hormonal imbalances – Inadequate levels of hormones such as progesterone can affect the result of implantation. The fluctuations in hormone levels can lead to the failure of IVF cycle.
- Lifestyle choices – If you are following unhealthy practices like smoking, drinking alcohol, or illegal drugs. Then such lifestyle choices can adversely affect the outcome of IVF treatment.
- Unexplained factors – At times, in some cases, it gets difficult to detect the exact cause of the failed IVF cycle. Infertility is a complex issue with various contributing factors if you suffer from any comorbidities.
- Ovarian dysfunction – Sometimes, medicines that are given to stimulate the ovaries for egg production fail to show any positive outcome. Therefore, the retrieved eggs may not be of optimal quality for fertilization and may negatively impact the process of the IVF cycle.
What Should I Avoid After IVF?
There are some precautions and lifestyle decisions to consider in order to maximize your chances of success after undergoing IVF treatment. Here are some things to avoid in general:

- Strenuous exercises may have an impact on implantation success or raise the risk of problems. Light to moderate exercise, such as walking or gentle yoga, can be useful. Therefore, one should avoid strenuous physical activities or workouts that place undue strain on the body.
- It is advised to avoid drinking alcohol and smoking during IVF treatment. Both consumption of alcohol and smoking cigarettes can harm fertility and raise the chance of problems during pregnancy.
- Caffeine use should be limited throughout IVF and pregnancy. For particular caffeine usage recommendations, consult your healthcare professional. Because excessive intake of caffeine has been linked to decreased fertility and an increased chance of miscarriage.
- Avoid heavy lifting or carrying anything that requires significant physical effort, since this can strain your abdominal muscles and potentially interfere with the implantation process.
- Putting your body in hot baths, saunas, or hot tubs can raise your core body temperature. Elevated body temperatures may impede embryo implantation. These activities are often discouraged throughout the IVF treatment.
- High levels of stress can negatively affect fertility and IVF success. While it’s hard to eliminate stress completely, managing it with techniques like deep breathing, meditation, or relaxing activities is crucial.
- It is recommended that you avoid sexual intercourse after embryo transfer as part of the IVF process unless your healthcare practitioner advises otherwise. Sexual activity during this time period may disrupt the implantation process.
Are There Any Complications With IVF?
IVF is a complex procedure but it is safe, effective, and performed with modern assisted reproduction technology. Though, it is important to know that with every treatment, there are certain potential complications and risks involved. Here are a few risks that are associated with IVF treatment:
- Ectopic pregnancy – It usually occurs when the fertilized egg gets implanted outside of the uterus instead of getting implanted into the inner uterine lining. Ectopic pregnancy can be fatal in some cases, therefore, it is always advisable to get immediate medical assistance for the same.
- Multiple pregnancies – At times, IVF treatment increases the chances of multiple pregnancies, such as twins, triplets, or more. Also, it involves a higher risk of complications for both babies and the mother. Multiple pregnancies can result in low birth weight, developmental issues, and premature birth.
- Ovarian hyperstimulation syndrome (OHSS) – It is a condition, in which the ovaries become painful and swollen as side effects of the given medication for healthy egg production. Though the early stages of OHSS can be resolved on their own, in rare cases they can become worse and may require medical intervention.
- Failed implantation – It is important to note that not all IVF cycles are successful. It happens because of the failed fertilization and implantation of the cultured embryos. The most common reasons for failed implantation are that the sperm fails to penetrate the egg or that there is no viable egg formation for embryo culture.
- Ovarian torsion – It is one of the rare but critical conditions in which the ovaries tend to twist, potentially cutting off their blood supply. This condition generally requires immediate surgical intervention in order to untwist the ovary and resume blood flow.
- Depression – The whole process of IVF can be burdensome for some patients and can take a toll on their psychological health. IVF treatment can be very demanding, emotionally draining, resulting in anxiety and depression.
It is always suggested that you discuss all the risks and complications with your fertility specialist beforehand to avoid any unexpected situations that can stress you out. By becoming aware, you will be able to figure out the early signs of any sort of risk or complications and inform your specialist timely.
Side Effects of IVF Injections

Injections are given during IVF treatment to stimulate the ovaries in order to produce healthy eggs for fertilization. The common IVF injections and fertility drugs that are given during the first few steps of the procedure are clomid, letrozole, gonadotropins, lupron, and more, according to the requirements. The quality and dosage of fertility drugs may vary from one individual to another based on their fertility requirements. Some of the side effects that patients may experience after IVF injections are:
| Type of fertility drug | Potential side effects |
| Clomid |
|
| Letrozole |
|
| Lupron |
|
| Gonadotropins |
|
How Do I Select an IVF Clinic in India?
It is always the best idea to look for the best IVF clinic in India before going to any random fertility clinic. To find or select the best IVF clinic in India, one should consider several factors. Here are some factors that can help you make an informed decision for yourself and will also help you prepare better for the treatment –
- Research for information – You can always conduct thorough research in order to find out the best IVF clinic in India. As you are planning to take an important step in your life, it is necessary to look for a clinic with a good track record, a better success rate, and a good reputation. Also, you can always see the reviews, ratings and patient testimonials of the selected clinic to get knowledge about the facilities through their experiences.
- The expertise of the specialist – Shortlist clinics that have highly qualified fertility specialists who have a good record of experience and expertise in their career as fertility consultants.
- Infrastructure – IVF clinics equipped with advanced technology and built with modern infrastructure always provide safe and effective fertility treatments. This can greatly impact the chances of a successful IVF treatment.
- Patient care – IVF treatment or any sort of fertility treatment can be emotionally draining and exhausting for some patients. Therefore, it is always a good idea to consider how well the clinic is offering care to patients who are undergoing treatments.
- Location of the clinic – Check the location of the clinic to note its accessibility from your residence. This can help you make your treatment journey smoother.
- Phone consultation – After shortlisting IVF clinics, you can select the most favourable one. Later, you can always schedule a phone consultation before visiting the clinic.
- Range of services – Also, check the range of fertility services the chosen clinic is offering, including diagnostic tests, fertility counseling, and genetic screening. This will help you avail services under one roof rather than going to different locations for the required services.
- IVF treatment cost– Enquire about the cost of IVF offered by the shortlisted clinic. You can always ask them about payment options, insurance coverage, and any available treatment package programs.
What Questions Can You Ask Your Fertility Specialist?
Here are a few general questions you can ask your fertility specialist to get an idea of the IVF treatment before undergoing it:
- Why am I unable to conceive a baby naturally?
- Are there any alternative methods aside from IVF?
- What should I eat and avoid during IVF treatment?
- Is IVF treatment very demanding?
- What are the benefits of IVF treatment?
- Can I go to the gym during IVF treatment?
- How much time does IVF treatment require?
- Is IVF treatment painful?
- What diagnostic tests are included in IVF treatment?
- What is the cost of IVF treatment?
- What is the success rate of IVF treatment?
Conclusion
IVF is a renowned assisted reproductive technology (ART) that has been helping many couples and individuals in need to achieve their fertility requirements. The above article gives you detailed information about the IVF treatment, from what it is to diagnoses, to side effects, and covers many other important aspects that are necessary to know. If you still have any concerns and want to know more about IVF treatment, call us or book an appointment with us for a free consultation.
FAQs
I am 45, can I still undergo IVF treatment?
If you are not experiencing menopause, you can always undergo IVF treatment to try your chances.
How long does it take IVF to show results?
Experts say that you can take the pregnancy test after 8–10 days of IVF treatment. If it shows a positive sign, that means it is a confirmed pregnancy.
Can I conceive through IVF after menopause?
Menopause is considered an ovarian failure, and the female body stops the production of viable eggs. Therefore, it is difficult to conceive through IVF treatment after menopause.
How long do I have to take off from work for the IVF procedure?
It is said that one can resume work one or two days after the IVF procedure after taking proper rest. However, the condition may differ from one patient to another, so it’s better to consult your doctor about it to get an accurate timeline for resuming work.
Is IVF treatment stressful?
IVF treatment can be stressful for some and can turn out to be emotionally and physically draining. However, it can be managed by joining groups and telling friends and family about the treatment to get the required support.
What is the full form of IVF?
IVF is the acronym for In vitro fertilisation. It is the process of fertilisation of an egg with sperm outside the body in a carefully controlled environment and then transferring the embryo (fertilised egg) into the uterus of the gestational carrier (female partner or surrogate).
How many injections are needed in an IVF cycle?
Many patients wonder how many fertility medication injections will be needed during the IVF cycle. There is no definite number. The frequency and dosage of medications depend entirely on the IVF plan specific to your age, reproductive health, and the health of your ovaries. This can range from 10-12 days of injections during the IVF cycle.
What are the benefits of IVF?
IVF is one of the preferred forms of ART (artificial reproductive technology) especially for specific causes of infertility. In the IVF procedure, the healthiest sperm and egg are chosen for fertilisation, post which the healthiest embryo is selected for implantation, thus increasing your chance of having a healthy baby.
When should I opt for IVF?
Couples unable to conceive even after timed intercourse (coinciding with ovulation) and hormonal therapy can consider IVF, especially if IUI (intrauterine insemination) proved unsuccessful.
How many IVF cycles should a woman try?
On average, a woman should try for two to three IVF cycles, but only after consulting well with your fertility expert.
Our Fertility Specialists
Related Blogs
To know more
Birla Fertility & IVF aims at transforming the future of fertility globally, through outstanding clinical outcomes, research, innovation and compassionate care.
Had an IVF Failure?
Talk to our fertility experts

 Our Centers
Our Centers