Difference Between Tubectomy and Vasectomy

Table of Contents
There are many couples who choose to opt for permanent birth control. It can be because of many personal reasons. We understand that it is a big decision; hence, one must understand all the options available.
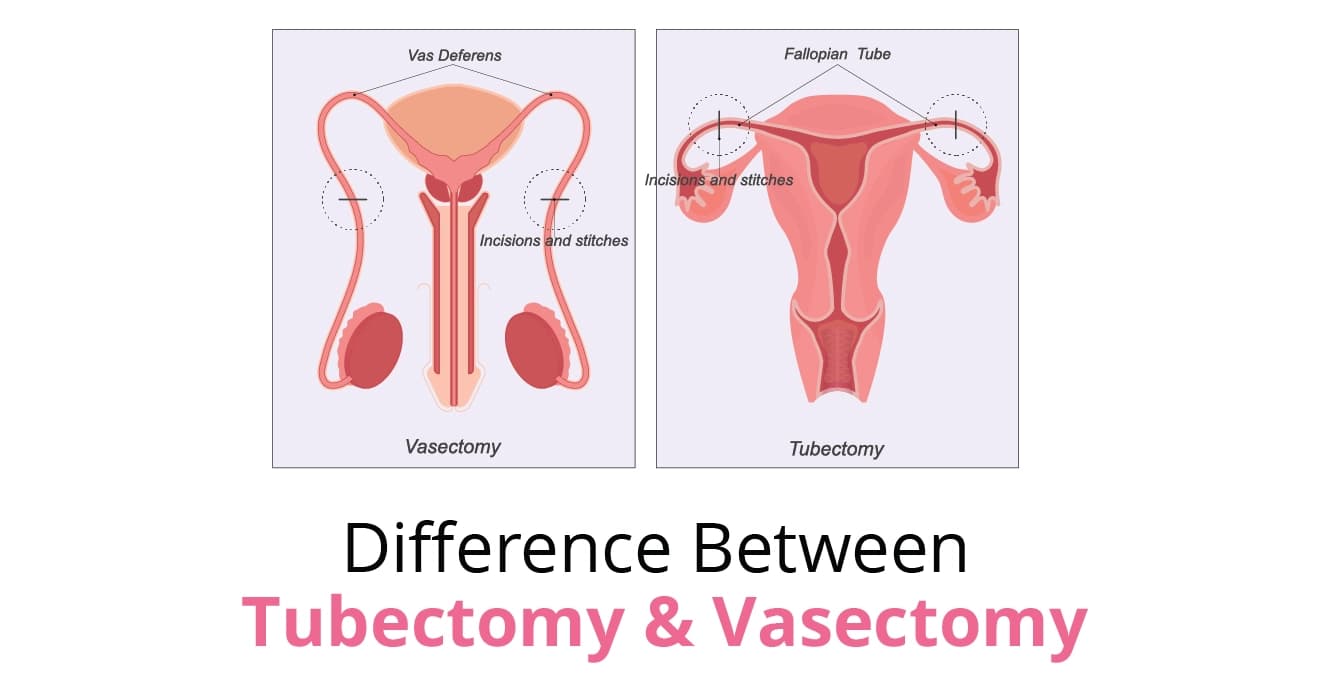
When you look for medical terms related to permanent birth control, tubectomy, and vasectomy pop up. While both are effective methods, they differ significantly in terms of procedure, recovery, and who undergoes the surgery.
This blog will make you understand the difference between tubectomy and vasectomy, and clear all the common myths to help couples make a confident and informed choice together.
What is a Vasectomy and Tubectomy?
For men, a vasectomy is a permanent method of birth control. In order to prevent sperm from entering the semen, a straightforward operation is used to block the tubes known as the vas deferens, which transport sperm from the testicles to the urethra.
Sexual function and the ability to ejaculate are unaffected by a vasectomy. The body merely reabsorbs the sperm while the testes continue to manufacture testosterone and other male hormones. It’s crucial to remember that it doesn’t provide defence against STIs.
Although reversal surgery is occasionally feasible, it does not ensure fertility restoration. Therefore, before choosing to have a vasectomy, it is essential to carefully study the operation.
Tubectomy is a method of permanent birth control for women, where, in order to stop eggs from entering the uterus for fertilisation, specialists cut, tie, or seal the fallopian tubes.
Tubectomy does not affect a woman’s hormones, menstrual cycle, or sexual function, and is considered a safe and effective permanent contraceptive option when family planning is complete.
Understanding vasectomy vs tubectomy helps couples choose the option that best aligns with their medical needs and long-term family planning goals.Let’s get into details.
Difference Between a Vasectomy and a Tubectomy
|
Aspect |
Vasectomy |
Tubectomy |
|
Who undergoes the procedure |
Male partner |
Female partner |
|
What it is |
A surgical procedure that blocks or cuts the vas deferens |
A surgical procedure that blocks or cuts the fallopian tubes |
|
Purpose |
Prevents sperm from mixing with semen |
Prevents the egg from reaching the uterus |
|
Type of procedure |
Minor, minimally invasive |
Major surgery (often laparoscopic) |
|
Anaesthesia |
Local anaesthesia |
General or spinal anaesthesia |
|
Duration of procedure |
15–30 minutes |
30–60 minutes |
|
Hospital stay |
Usually not required |
Day care or short hospital stay |
|
Recovery time |
2–3 days |
1–2 weeks |
|
Pain and discomfort |
Mild |
Moderate |
|
Effectiveness |
Over 99% effective |
Over 99% effective |
|
Impact on sexual function |
No impact |
No impact |
|
Reversibility |
Sometimes reversible (not guaranteed) |
Generally irreversible |
|
Risk and complications |
Low risk |
Slightly higher risk due to surgery |
|
Cost |
Lower |
Higher |
Process of Vasectomy
Tubectomy and vasectomy differ in their steps. The vasectomy procedure is performed as follows:
- The scrotum and vas deferens are first numbed by giving local anaesthesia.
- The doctor then makes a small incision in the upper part of the scrotum and accesses the vas deferens.
- Both vas deferens are then cut, tied, and sealed to prevent the passage of sperm.
- Cutting and tying, cauterisation (sealing with heat), or using clips are the common methods used for this step.
- The procedure usually takes only 25-30 minutes. This also becomes the main difference between tubectomy and vasectomy.
- There is also a less invasive non-surgical technique. In a ‘no scalpel’ method, the doctor searches for the ductus deferens under the skin of the scrotum. He then holds it in place with a small clamp.
- Then, an instrument is used to make a tiny hole in the skin and stretch the opening. Here, the vas deferens are cut and tied.
- The procedure involves a smaller opening, less tissue trauma, and provides quicker recovery.
Process and Effects of Tubectomy
Most of the steps of tubectomy and vasectomy are similar. However, the general steps followed in tubectomy are:
- Tubectomy is performed in a hospital or outpatient surgical clinic under general anaesthesia.
- One or two small cuts are made in the abdomen, and a laparoscope is inserted.
- This instrument cuts, ties, or seals the fallopian tube.
- Cut and tie: The surgeon cuts a section of the tube and ties or clips both ends.
- Cauterisation: Heat is used to seal the tubes shut.
- Tubal rings or clips: Small devices are placed around the tubes to block them.
- The skin incisions are then closed with stitches. The patient is discharged within a few hours after the procedure.
- Doctors also prefer tubectomy immediately after childbirth. They do it via a small incision near the navel or during caesarean delivery.
- Like a vasectomy, tubal ligation does not protect against STDs, including HIV.
Effectiveness of Vasectomy
- Over 99% effective in preventing pregnancy
- Becomes effective only after semen is confirmed sperm-free (usually after 8–12 weeks)
- Considered one of the most reliable permanent contraception methods
- Failure rate is less than 1%
Effectiveness of Tubectomy
- Also, over 99% effective
- Provides immediate protection once the procedure is completed
- Long-term failure rate is very low, but slightly higher than vasectomy
- Effectiveness depends on surgical technique and healing
Recovery Time
Vasectomy
- Most men resume daily activities within 2–3 days
- Mild swelling or discomfort may occur for a few days
- Strenuous activity and sexual intercourse are usually avoided for about one week
Tubectomy
- Recovery typically takes 1–2 weeks
- Abdominal soreness, fatigue, or mild pain is common
- Heavy lifting and strenuous activity should be avoided during recovery
- Full recovery may take longer if performed after childbirth or via caesarean section
Impact on Overall Health
- Neither vasectomy nor tubectomy affects hormone levels
- Sexual desire, performance, and pleasure remain unchanged
- Men continue to produce testosterone after a vasectomy
- Women continue normal menstrual cycles after a tubectomy
- Neither procedures cause long-term weakness or health problems
- They only prevent pregnancy and do not interfere with normal bodily functions
Risks
Vasectomy Risks
- Mild pain, swelling, or bruising
- Infection at the incision site (rare)
- Temporary discomfort during ejaculation in a few cases
- Very low risk of failure or reconnection of the vas deferens
Tubectomy Risks
- Risks associated with general anaesthesia
- Infection or bleeding
- Injury to nearby organs (rare)
- Slightly increased risk of ectopic pregnancy if failure occurs
Conclusion
Both vasectomy and tubectomy are highly effective and reliable methods of permanent contraception. However, vasectomy is a simpler, safer, and less invasive procedure with quicker recovery and fewer risks compared to tubectomy. While both partners can choose either option, vasectomy is often medically preferred when suitable. The decision should be made after careful discussion between partners and consultation with a healthcare professional to ensure it aligns with long-term family planning goals.
FAQs
What is the recovery time of a vasectomy & tubectomy?
The recovery time of a vasectomy is less compared to a tubectomy. On one hand, after a vasectomy, men can return to their normal routine within a week; it takes almost 2 weeks for women to recovery after a tubectomy.
What are the risks associated with vasectomy & tubectomy?
Post-vasectomy can cause mild pain, swelling, or bruising. You can also risk developing an infection at the incision site, which is a rare occurrence. Likewise, post-tubectomy, women face risks associated with general anaesthesia. This process can also cause infection or bleeding, as well as a risk of injury to nearby organs.
Our Fertility Specialists
Related Blogs
To know more
Birla Fertility & IVF aims at transforming the future of fertility globally, through outstanding clinical outcomes, research, innovation and compassionate care.
Had an IVF Failure?
Talk to our fertility experts

 Our Centers
Our Centers




















